Invisible Impairment: The Silent Saboteur of Daily Life

Picture this: you’re watching a film you’ve been waiting to see for months. The visuals are stunning, the soundtrack perfect — but every few minutes, the screen glitches. Just a second here and there, yet enough to break the flow. You reach the end, but something never quite connects. That’s what fragmented sleep feels like: the story runs, but the rhythm is lost. The numbers flashing on your tracker can insist you’ve had a full night’s sleep – the hours add up, the data looks fine. Still, you wake up with the nagging sense that something was missing. The result? Sleep that looks whole on paper — or at least in the data — but in reality can be anything but that.
The problem might look small, but its impact can be anything but. And it reveals something unsettling: we only start taking sleep problems seriously once they’ve become serious enough to earn a label. Why do we have to wait until things get bad before anyone listens? Why do our healthcare, insurance, and social habits make it so hard to act sooner — before exhaustion becomes the norm?
Making the Invisible Visible: Defining the Grey Zone of Sleep
You know that feeling when you should be fine — your wearable says you slept well, your doctor isn’t worried — yet you still wake up tired, foggy, and not quite yourself? You’re not imagining it. You might be living in that in-between space where sleep looks “normal” on your wearable but doesn’t feel restorative in real life. Sometimes your wearable looks fine and your questionnaire scores don’t cross a cutoff — so on paper nothing’s wrong, even when your days say otherwise. And when your concerns get brushed aside, it’s easy to start second-guessing yourself, wondering if it’s all in your head. But it’s not. What you feel is real, and it matters.
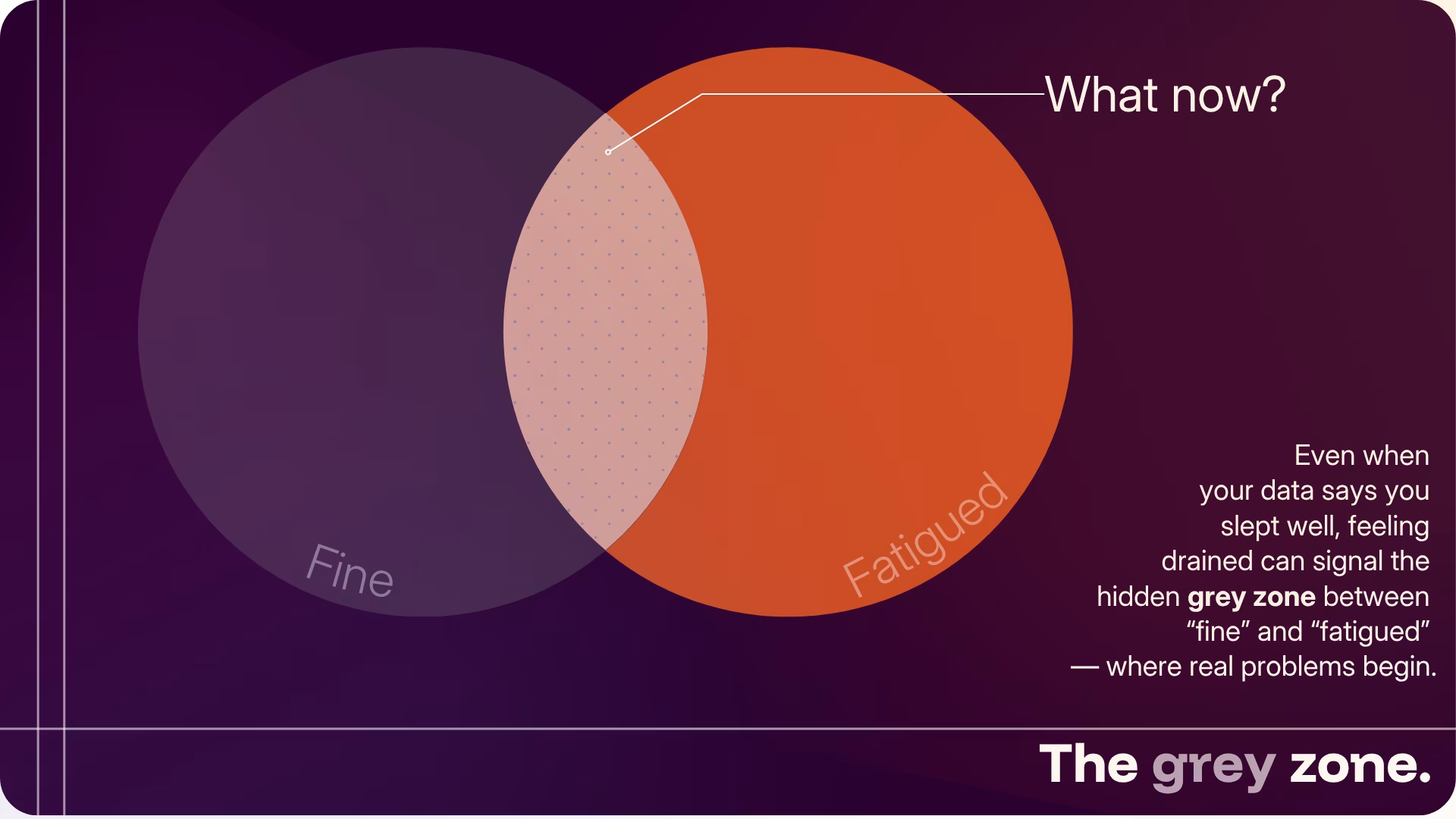
Part of the problem is that poor sleep has become the norm. Between work, family, and endless to-dos, exhaustion is almost expected: rest is almost a luxury, not a need. But the issue goes deeper. Our healthcare systems are built to react only when symptoms cross a line. If you don’t “tick enough boxes,” you’re told you’re fine, even when your daily life says otherwise. The same happens in mental health — you can meet a few criteria for low mood fatigue or even depression and still be left without help. Sleep struggles fall into the same trap.
And this is exactly where attention is most needed. The goal isn’t to label you as unwell — it’s to make sure you don’t have to shrug off the early signs that something’s off, or second-guess what your body’s trying to tell you. Recognising those early signals isn’t just self-care; it’s how you protect your focus, your energy, your long-term wellbeing — and, most of all, the people who rely on you.
This is what we mean by invisible impairment: a gap between what technology measures and what people actually feel — when sleep appears normal in the data, yet fails to restore how you function, think, and feel.
Sleep Fragmentation: The Subtle Cuts that Steal your Rest
Sleep fragmentation happens when your night is broken into tiny awakenings you may never remember. Each interruption might be small, but together they chip away at the continuous rest your brain and body need to truly restore themselves. It’s like watching a film that keeps skipping frames — the story still plays, but the flow breaks, and the feeling never fully lands.
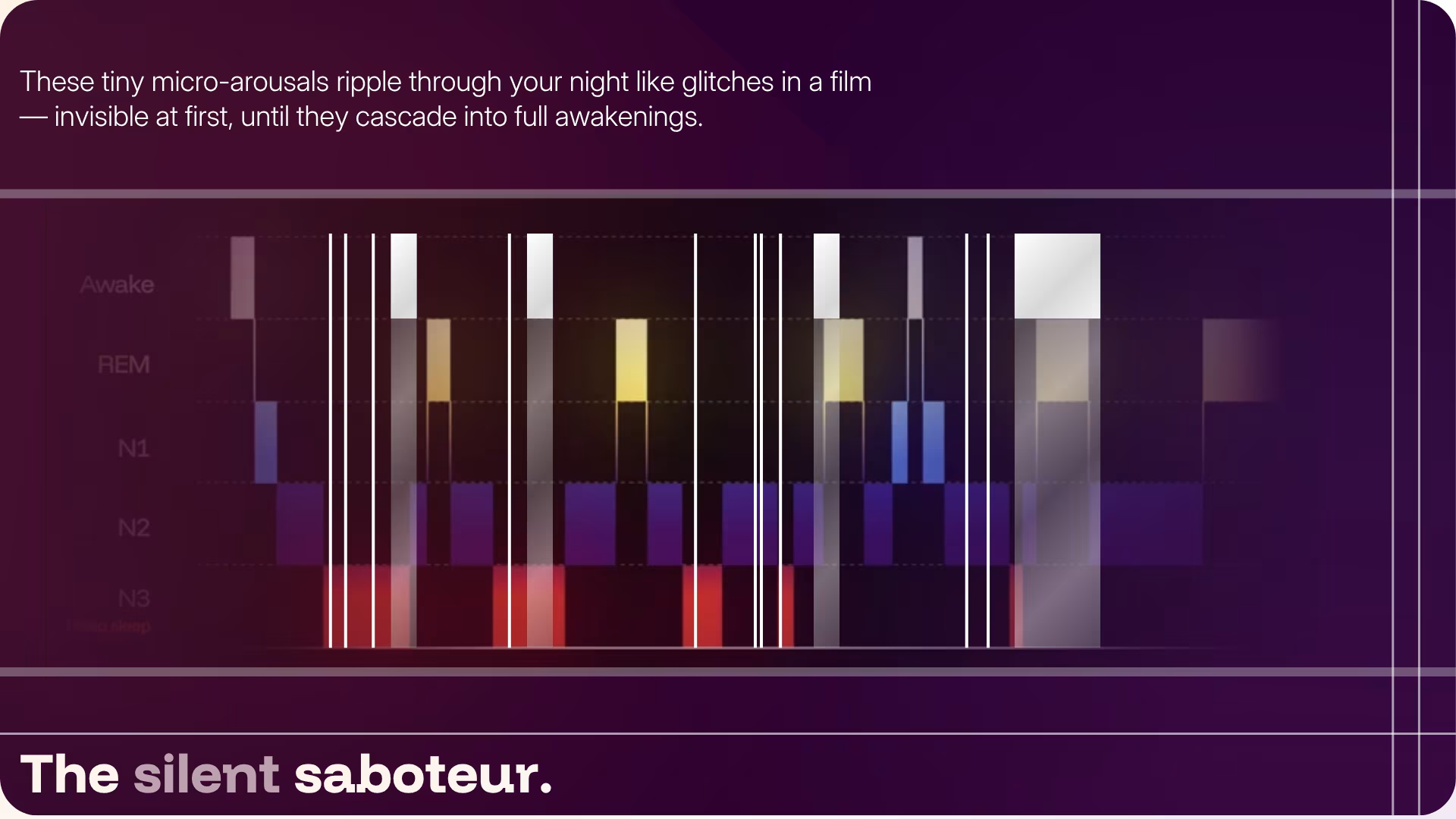
What makes fragmentation tricky is that it doesn’t require a diagnosis to appear. Pain, stress, or even an ordinary night can trigger micro‑arousals that leave sleep lighter, shallower, and far less refreshing 1. And it doesn’t stop there — a warm room, your partner shifting beside you, or a mind that just won’t quiet down — can do the same. These are everyday moments we rarely think twice about, yet they can quietly chip away at the kind of deep, uninterrupted rest the body depends on. The same pattern shows up in insomnia, where fragile REM cycles interrupt the brain’s nightly work of sorting memories and emotions 2.
If you’ve had fragmented sleep before, you likely wouldn’t describe it as just “waking up.” It feels more like never really sinking deep. And science backs this up: fragmented nights are linked to poorer subjective sleep quality and higher rates of depressive symptoms, both in clinical and community samples 3. But it doesn’t stop there—research shows these sleep disturbances can even drain the brain’s capacity to metabolize energy, underscoring just how fragile restorative sleep really is 4.
The challenge is that fragmentation often goes unnoticed by the very tools designed to track our sleep. These disruptions remain hidden, quietly eroding restfulness night after night — while everything still looks fine.
The Real Price of Broken Nights
When your sleep is cut into pieces, the damage doesn’t end when morning comes. It seeps into your day — quietly at first, then all at once.
- Your mornings no longer feel satisfying: you feel groggy even after a seemingly full night
- Your mood takes a punch: you find yourself feeling irritable or moody more often
- Your cognitive capacity slows down: you find everyday tasks harder, slips in focus become more common, and your reaction times drop.
Over time, fragmented sleep has been associated in studies with changes in cardiovascular, metabolic, and emotional health markers — suggesting that the quality of rest may influence more than how refreshed we feel in the morning.
Think of it like using a broken charger. You expect your phone to charge overnight, but wake up to realize that it hasn’t even reached 40%. The charger only lets current in intermittently, almost like a broken night of sleep. Your phone might still turn on, but it won’t last you for the whole day.
That’s the daily cost of these interruptions: you think you’ve recharged overnight, but wake up to realize you’re running on half power.
Tracking Sleep That Truly Matters: What Current Tools Miss
If you’ve ever been told your sleep is “normal” because you clocked eight hours, you’ve already met the limits of diagnostic thresholds. Traditional healthcare systems divide people into tidy categories — unwell or well — but sleep doesn’t work that way. Many of us live in the grey zone: not meeting clinical criteria for a disorder, yet far from experiencing truly restorative sleep.
For decades — and long before wearables and sleep scores — most of us grew up with the same advice from our parents: “Get your eight hours.” It was simple, and it still matters. But as science has caught up, we’ve learned that the old rule is only part of the story. More recent guidance from the National Sleep Foundation recognises that hours alone don’t define good sleep. Wearables now try to add nuance by estimating stages and patterns — progress, but still far from capturing the full picture. The real difference between a night that restores and one that drains is continuity — something far harder to measure.
"The real difference between a night that restores and one that drains is continuity — something far harder to measure."
And that’s exactly what today’s wearables often miss — the subtle disturbances people can feel but consumer data rarely captures, from micro-arousals to changes in K-complex prevalence, sleep spindle density, and brain-wave power. Most wearable consumer sleep trackers offer a glimpse into sleep architecture, but mostly rely on indirect signals like heart‑rate variability or movement. Useful as these can be, they rarely pick up the tiny awakenings that fragment a night. The result? A sleep score that looks reassuringly normal, even when your night feels anything but.
"The result? A sleep score that looks reassuringly normal, even when your night feels anything but."
And while a handful of early adopters and biohackers now buy consumer EEG headbands, most of those devices still lack the sensitivity or validation needed to detect the subtler forms of sleep disruption. The result is the same gap: what people feel and what the data shows don’t yet line up.
The good news is that sleep technology is evolving fast. Smarter wearables, near-EEG headbands, and contactless sensors are becoming more widely available, inching closer to what’s needed for truly personalised sleep insights. Big-tech and health innovators are now creating solutions that could finally help people who fall between “well” and “unwell” — those whose sleep looks fine in your sleep score but doesn’t feel that way. Yet progress remains slow, weighed down by challenges like reimbursement, validation, and data integration.
What’s clear is that we need to act much earlier — not only to stop small issues from deepening, but to shift our focus from simply extending life to preserving the quality and vitality of it.
What This Means for Deep Sleep Technologies
Invisible impairments are not minor annoyances, but real warning signs. Left unaddressed, they potentially could shorten our health span, brain health and most significantly reduce our quality of life. At Deep Sleep Technologies we believe the future of sleep health is not about waiting for decline. It’s about stepping in sooner rather than later, and addressing problems in a preventative, continuous, and long-term way.
This means:
- Detecting the hidden sleep disruptions that today’s wearables and conventional metrics often miss
- Responding and Intervening in real time, when a change in trajectory is still possible
- Helping each person realign with their natural rhythm — so recovery becomes continuous, not occasional
Our mission is clear: to detect what others can’t and restore what biology was designed to do — transforming sleep from a passive state into the foundation of prevention, resilience, and restored vitality.
References
[1] Bonnet, M. H., & Arand, D. L. (2003). Clinical effects of sleep fragmentation versus sleep deprivation. Sleep Medicine Reviews, 7(4), 297–310. https://doi.org/10.1053/smrv.2001.0245
[2] Feige, B. (2023). Insomnia and REM sleep instability. Journal of Sleep Research. Advance online publication. https://doi.org/10.1111/jsr.14032
[3] Wu, D., Tong, M., Ji, Y., Ruan, L., Lou, Z., Gao, H., & Yang, Q. (2021). REM sleep fragmentation in patients with short-term insomnia is associated with higher BDI scores. Frontiers in Psychiatry, 12, 733998. https://doi.org/10.3389/fpsyt.2021.733998
Pesonen, A. K., Gradisar, M., Kuula, L., Short, M., Merikanto, I., Tark, R., Räikkönen, K., & Lahti, J. (2019). REM sleep fragmentation associated with depressive symptoms and genetic risk for depression in a community-based sample of adolescents. Journal of Affective Disorders, 245, 757–763. https://doi.org/10.1016/j.jad.2018.11.077
[4] Stamatakis, K. A., & Punjabi, N. M. (2010). Effects of sleep fragmentation on glucose metabolism in normal subjects.Chest, 137(1), 95–101. https://doi.org/10.1378/chest.09-0791